Most women should get screened for breast cancer every other year starting at age 40, a decade earlier than previously recommended, according to draft guidelines issued Tuesday by a government-backed panel of experts.
The U.S. Preventive Services Task Force said its new guidance could save 19% more lives.
Each year in the U.S., about 264,000 cases of breast cancer are diagnosed in women and roughly 2,400 in men, according to the Centers for Disease Control and Prevention. Around 42,000 women and 500 men in the U.S. die each year from the disease.
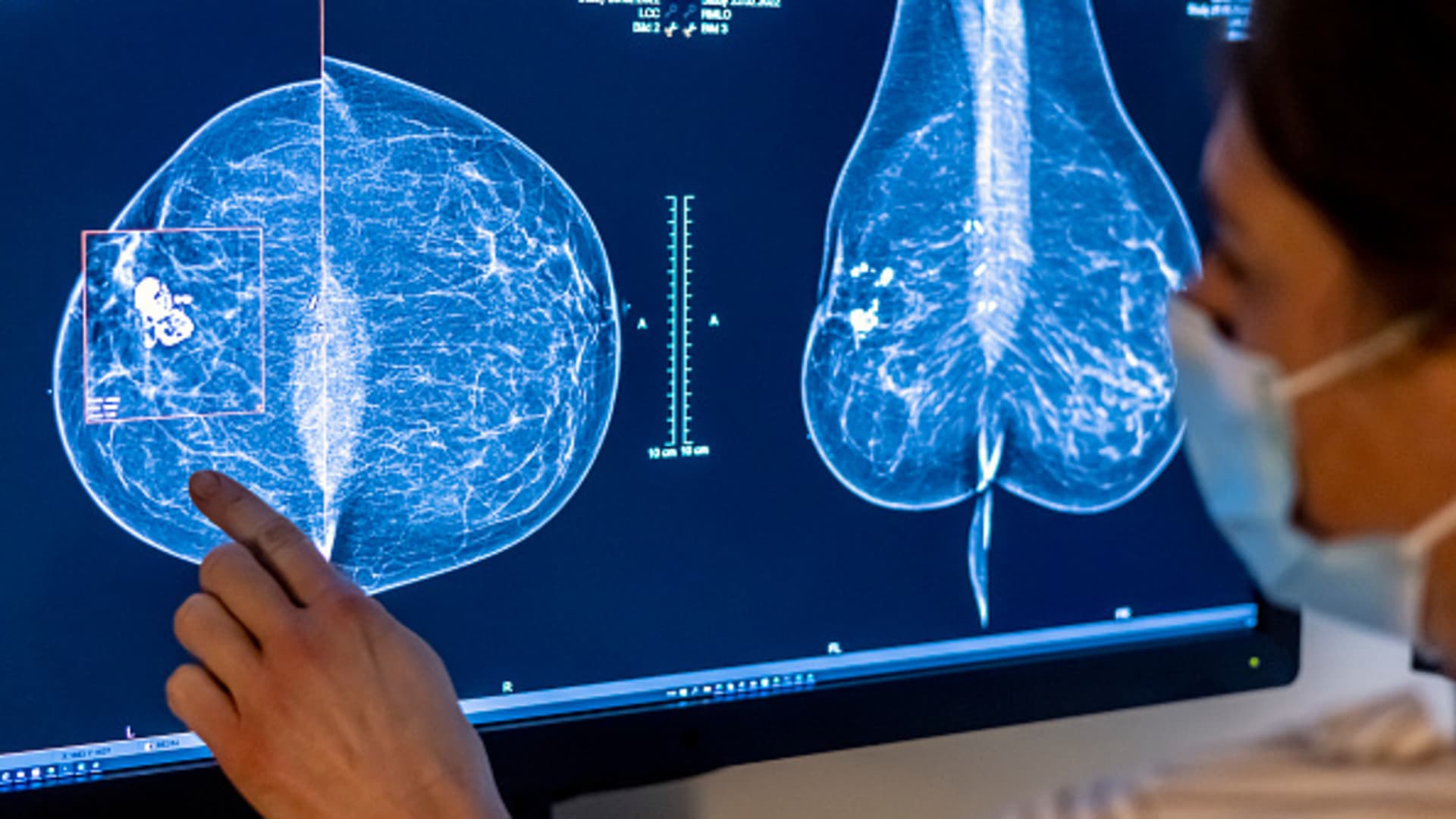
Breast cancer screenings typically involve a mammogram, which is an X-ray of the breast.
The panel’s guidance applies to cisgender women and all other people assigned female at birth who are at average risk of breast cancer. It does not apply to people at high risk of breast cancer, including those who have a family history of the disease.
The U.S. Preventive Service Task Force’s recommendations are usually widely adopted in the U.S. The panel’s previous guidance, which was last updated in 2016, suggested that women should start screening every other year at age 50.
That guidance also said women in their 40s could talk to their doctors about getting screened, particularly if they have a family history of breast cancer.
At the time, the panel was concerned that earlier screenings could lead to unnecessary treatment for younger women, including biopsies that turn out to be negative. A biopsy is a sample of tissue taken from the body, which gets tested for a disease like cancer.
But the panel said it changed that guidance due to “new and more inclusive science” about breast cancer in people younger than 50, said Dr. Carol Mangione, immediate past chair of the U.S. Preventive Services Task Force, in the guidelines.
The rate of breast cancer among women ages 40 to 49 increased by 2% each year on average from 2015 to 2019, according to the National Cancer Institute.
The panel said the new guidance also aims to ease the disparities in breast cancer death rates between Black women and white women.
Black women are 40% more likely to die of the disease than their white counterparts and “too often get deadly cancers at younger ages,” the panel said in the guidelines.
The panel “urgently” called for more research on how to eliminate the disparity.
“Ensuring Black women start screening at age 40 is an important first step, yet it is not enough to improve the health inequities we face related to breast cancer,” Dr. Wanda Nicholson, the panel’s vice chair, said in the guidelines.
Other medical groups, including the American College of Radiology and the American Cancer Society, already recommend annual breast cancer screenings before age 50.
Roughly 60% of women ages 40 to 49 reported having a mammogram within the past two years in 2019, according to the Centers for Disease Control and Prevention.